Chronic fatigue syndrome (CFS)
What's covered?


Chronic fatigue syndrome (myalgic encephalomyelitis) is a long-term neurological condition with many different symptoms. The most common one experienced is extreme tiredness. The good news is you can do many things to manage chronic fatigue syndrome — like cognitive behavioural therapy (CBT) and medication.
What is chronic fatigue syndrome?
CFS makes you feel exhausted and affects your mental function. You might have symptoms for a minimum of 3 months, significantly affecting your daily life.
Getting an early diagnosis is essential so you can begin to manage your symptoms and feel better.
What are the causes of chronic fatigue syndrome?
The exact causes of CFS are unknown, but research suggests it might be due to infections, problems with your immune system, and hereditary factors.
What are the symptoms of chronic fatigue syndrome?
CFS symptoms might differ daily, so it might be helpful to keep a diary and show it to your GP. You might also experience periods when your symptoms improve or worsen.
The most common symptoms of CFS are:
- feeling extremely tired all the time — this might affect your work performance and relationships
- problems sleeping — like waking during the night or still feeling tired in the day
- problems with your brain function (cognition) — like thinking, short-term memory, and concentration
- delayed recovery from physical activity (post-exertional malaise)
You might also have other symptoms, including:
- feeling sick or dizzy
- fast or irregular heartbeats (heart palpitations)
- flu-like symptoms — like a sore throat, headaches, and muscle or joint pain
If you’re experiencing any of these symptoms, you should see your GP. They might be able to rule out other health conditions presenting similar symptoms.
Find out more about how sleep affects your health.
How long does chronic fatigue syndrome last?
You might have CFS symptoms for a minimum of 3 months.
The symptoms of CFS can differ from person to person — this includes how long they last and the severity. Some people might recover faster, while others might have persistent symptoms for many years.
That’s why it’s important to see your GP if you notice any symptoms to start managing them and feeling better.
Is there a blood test for chronic fatigue syndrome?
There isn’t a blood test to diagnose chronic fatigue syndrome. Many health problems can cause the symptoms of CFS, so it’s important to see your GP to rule these out. Your GP will typically diagnose CFS by assessing your symptoms and medical history. You might also have blood and urine tests to help rule out other conditions causing your symptoms.
How to manage chronic fatigue syndrome
Unfortunately, CFS has no cure. But the good news is there are many things you can do to manage your symptoms and improve your quality of life. Management depends on how CFS affects you and will be tailored to your symptoms.
These include:
- practising good sleep hygiene — aim for 7-8 hours of sleep every night. Our magnesium supplements might also help improve your sleep quality
- cognitive behavioural therapy (CBT) — CFS isn’t a mental health condition, and CBT won't cure it, but it can help manage symptoms like pain and depression
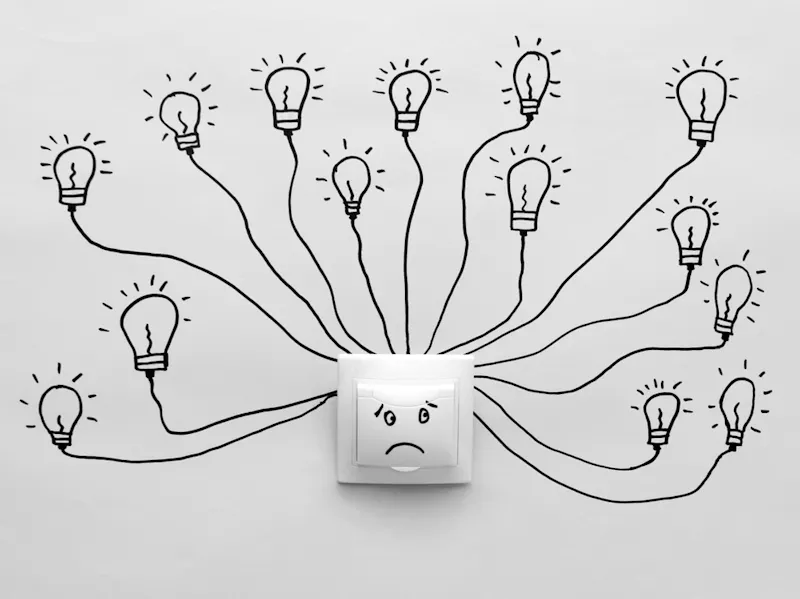
- pacing — a behavioural technique that helps you manage periods of activity and rest. This might include visualising your energy like a bank account, seeing periods of activity as ‘withdrawals’ and resting as ‘deposits’ into your account
- seeing a physiotherapist if you can include exercise into your management regime. But you shouldn't do this without the guidance of a specialist, as this might worsen your symptoms
- following a healthy diet — you should see a dietitian if you’re losing or gaining weight, or if you follow a restrictive diet
- getting referred to a specialist CFS service
Your GP might also give you advice about how to use the energy you have without making your symptoms worse. This might mean adapting your daily routine and lifestyle while your symptoms persist to help improve your quality of life.
Sapra A, Bhandari P. Chronic Fatigue Syndrome. [Updated 2022 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557676/
Wostyn, P. (2021). COVID-19 and chronic fatigue syndrome: Is the worst yet to come?. Medical hypotheses, 146, 110469.
The ME Association. ME/CFS. Retrieved 20 July 2022 from https://meassociation.org.uk/me-cfs-diagnosis/
National Health Service. Chronic fatigue syndrome. Retrieved 9 June 2022 from https://www.nhs.uk/conditions/chronic-fatigue-syndrome-cfs/