How Optimal Ranges Work: Thriva’s Approach
What's covered?

Even if your blood test results fall within the "normal" range, they might not be truly optimal for your health and longevity. Thriva’s optimal ranges are developed through a thorough review of the latest scientific research and clinical guidelines. These ranges are continually updated by our clinical team to ensure they reflect the best available evidence. Our goal is to provide more insight into your health by helping you see whether your results sit in ranges associated with the lowest risk of disease and mortality.
What are normal reference ranges?
Normal reference ranges are used to interpret your blood test results, determining whether your levels are considered "normal" or "abnormal". These ranges are based on values found in a ‘normal’ population, typically based on where 95% of a sample population falls.
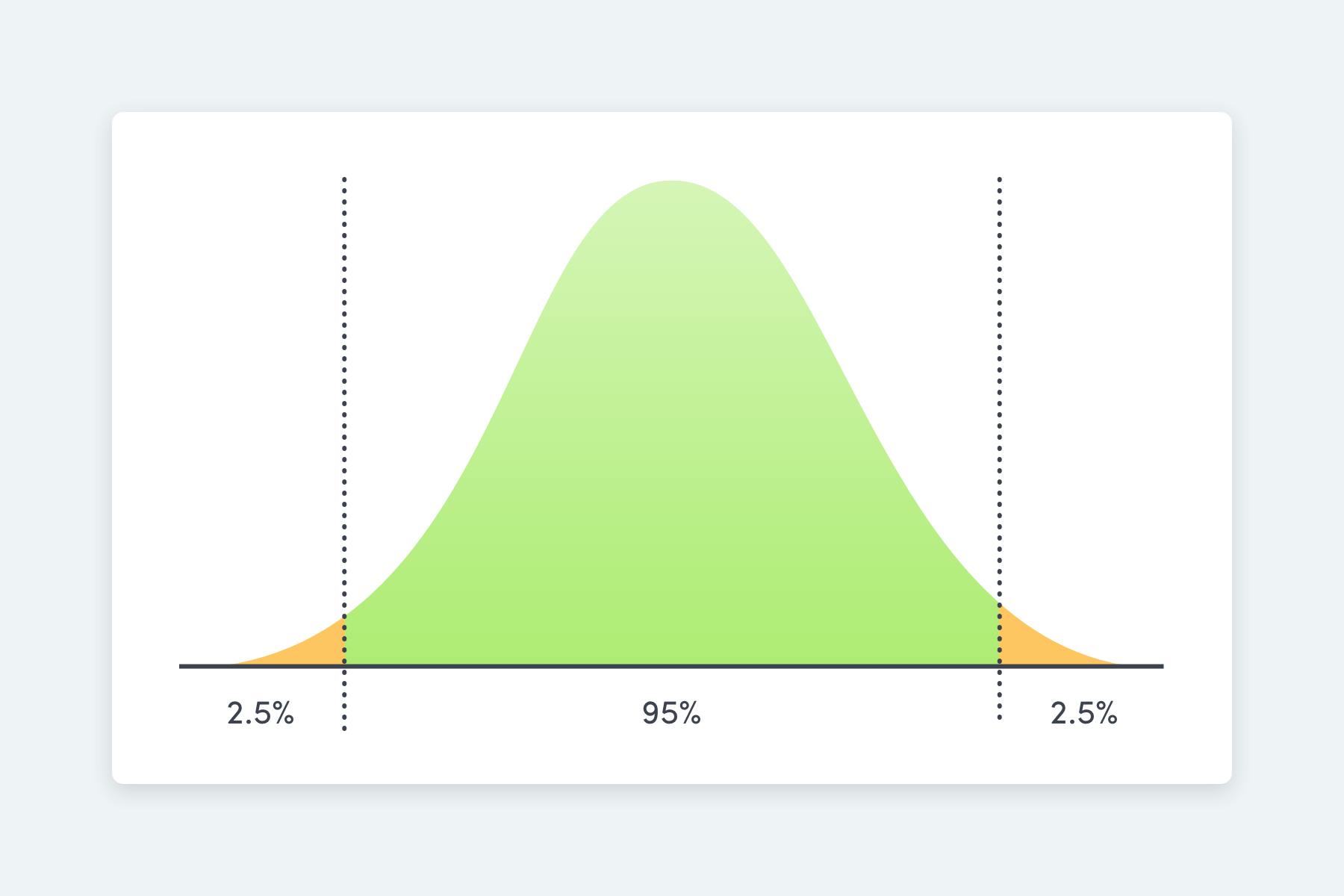
Some reference ranges are set based on evidence linking specific levels to an increased risk of certain health conditions. For example, cholesterol reference ranges are influenced by their association with heart disease risk.e.
Issues with normal reference ranges
There are several limitations to normal reference ranges:
- They often oversimplify the complex nature of health.
- They do not always consider the relationship between specific levels and disease risk or life expectancy.
- The research behind these ranges can rely on small sample sizes.
- Reference range populations might include individuals who are not entirely healthy, or who are at high risk of future disease.
Optimal reference ranges can help us overcome some of these limitations
What are optimal reference ranges?
At Thriva, we use a refined approach to establish optimal reference ranges. Our clinical team systematically reviews the latest scientific literature and clinical guidelines to identify ranges that are associated with improved health outcomes and longevity. This approach provides a more comprehensive understanding of your health beyond traditional reference ranges.
Optimal ranges are based on evidence linking specific levels of an analyte (a substance measured in a blood test) with a reduced risk of disease or enhanced life expectancy.
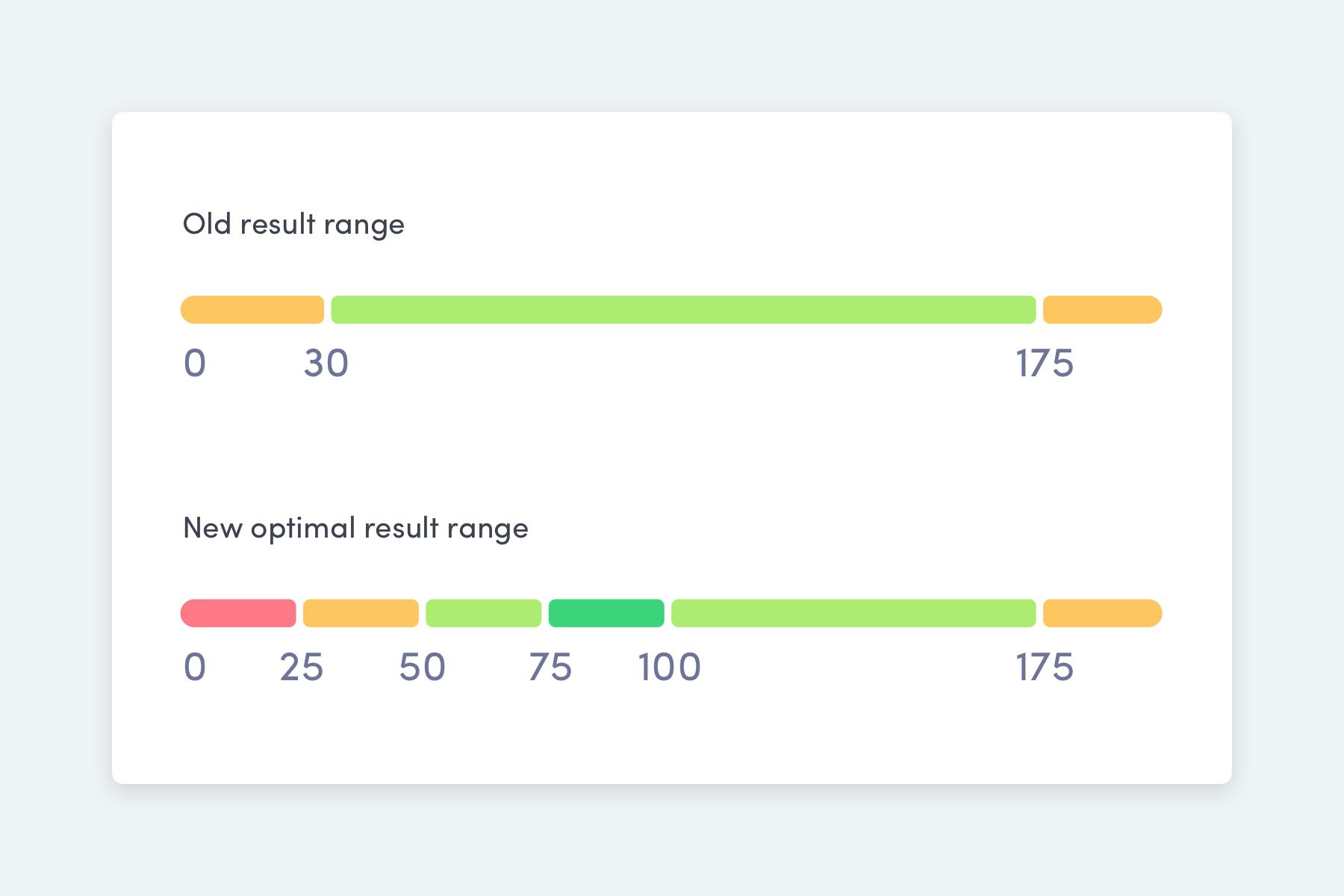
Take vitamin D as an example. Traditional vitamin D guidelines suggest that:
- Levels below 25 nmol/L indicate deficiency.
- Levels above 50 nmol/L are considered sufficient
This range is only based on the relationship between vitamin D, your bone health, and your risk of osteoporosis.
However, vitamin D is important for many other things, like your muscle and immune health. So the evidence suggests that the optimal range for vitamin D is actually between 75 nmol/L and 100 nmol/L — this is associated with the lowest risk of death (from all causes).
Understanding the Nuances of Optimal Ranges
It’s important to understand that optimal ranges are not always straightforward, and interpreting them requires a nuanced approach. While they are associated with better health outcomes, correlation does not always imply causation. Adjusting biomarkers to fit within these ranges does not automatically guarantee improved health, as the evidence can be complex and direct cause-and-effect relationships are not always clear. At Thriva, we base our recommendations on the most reliable evidence available.
Interpreting Optimal Ranges
Given these complexities, we don't suggest that targeting optimal levels for every biomarker is the only way to achieve better health and wellbeing. Instead, we encourage you to use optimal ranges as helpful guides to identify areas for improvement, while considering your overall health, lifestyle, and any existing medical conditions. Our doctors are here to provide personalised advice, tailored to your unique health needs and goals.
Summary
While normal reference ranges are useful for identifying clear abnormalities, they don’t always offer a complete picture of your health. Thriva’s optimal ranges provide a more refined perspective, helping you understand how your results align with the latest research on reducing disease risk and promoting longevity. At Thriva, we are dedicated to offering up-to-date, personalised insights to support you in making informed decisions about your health.
Kratzsch, J., Fiedler, G. M., Leichtle, A., Brügel, M., Buchbinder, S., Otto, L., ... & Thiery, J. (2005). New reference intervals for thyrotropin and thyroid hormones based on National Academy of Clinical Biochemistry criteria and regular ultrasonography of the thyroid. Clinical chemistry, 51(8), 1480-1486.
Petursson, H., Sigurdsson, J. A., Bengtsson, C., Nilsen, T. I., & Getz, L. (2012). Is the use of cholesterol in mortality risk algorithms in clinical guidelines valid? Ten years prospective data from the Norwegian HUNT 2 study. Journal of evaluation in clinical practice, 18(1), 159-168.
Sempos, C. T., Durazo-Arvizu, R. A., Dawson-Hughes, B., Yetley, E. A., Looker, A. C., Schleicher, R. L., ... & Dwyer, J. T. (2013). Is there a reverse J-shaped association between 25-hydroxyvitamin D and all-cause mortality? Results from the US nationally representative NHANES. The Journal of Clinical Endocrinology & Metabolism, 98(7), 3001-3009.
Spencer, C. A., Hollowell, J. G., Kazarosyan, M., & Braverman, L. E. (2007). National Health and Nutrition Examination Survey III thyroid-stimulating hormone (TSH)-thyroperoxidase antibody relationships demonstrate that TSH upper reference limits may be skewed by occult thyroid dysfunction. The Journal of Clinical Endocrinology & Metabolism, 92(11), 4236-4240.