Polycystic ovary syndrome (PCOS) is a condition that affects your ovaries — possibly affecting up to 1 in 10 women of reproductive age. The main features of PCOS are irregular periods, high levels of male hormones, and polycystic ovaries. This can make it harder for you to get pregnant and increase your risk of long-term health issues, like diabetes and heart disease. While PCOS can’t be cured, there are lots of things you can do to manage your symptoms and reduce your risks — like following a healthy lifestyle and medication.
What is PCOS?
PCOS is a collection of symptoms that affect your ovaries. It has three main features (if you have two out of three you might have PCOS):
- irregular periods — because you’re not ovulating
- high levels of “male hormones” — like testosterone
- polycystic ovaries — where fluid-filled sacs (follicles), containing immature eggs, grow in your ovaries
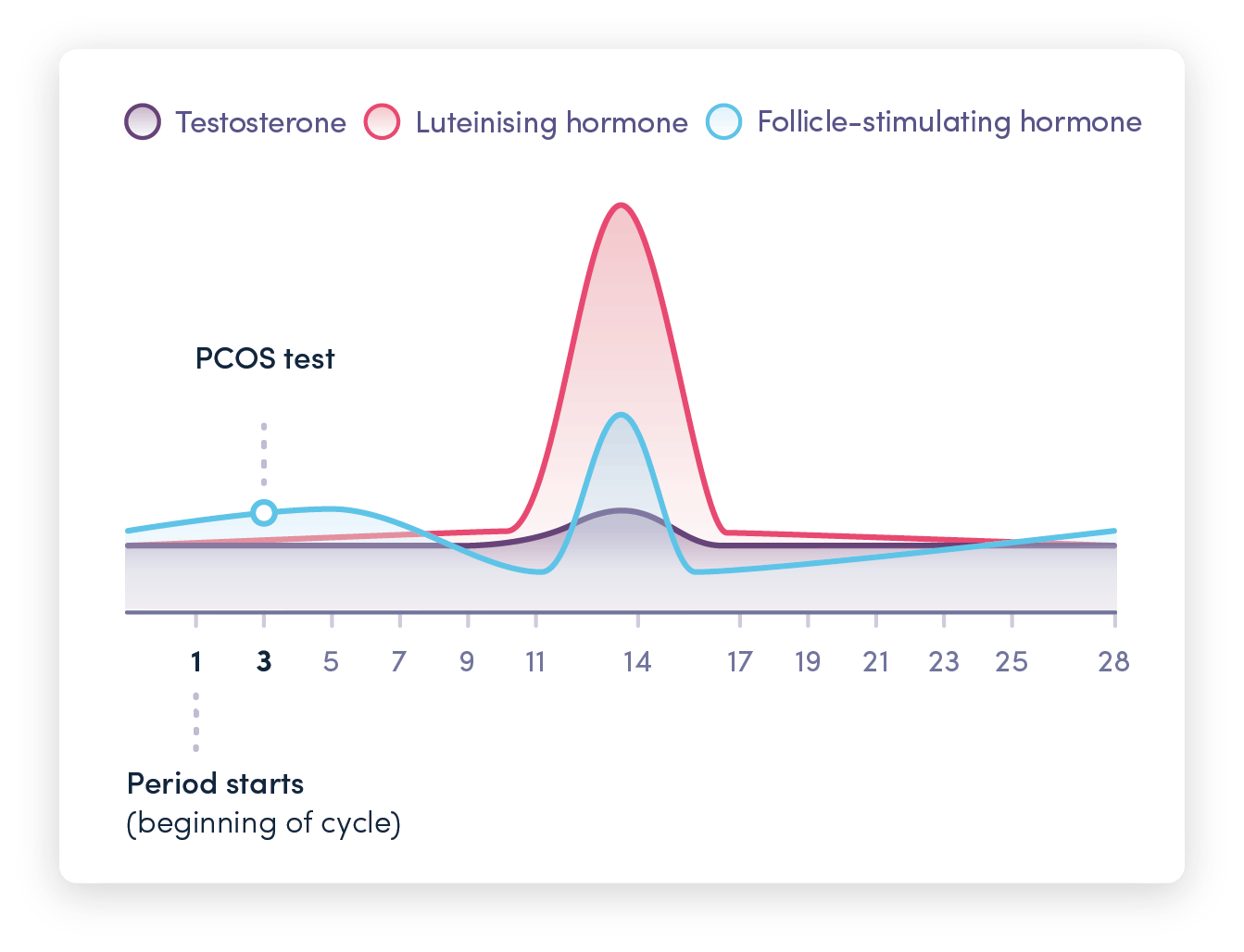
If you have PCOS, your follicles often don’t release an egg — meaning you don’t ovulate. This causes your oestrogen and progesterone levels to be lower than usual. It also affects your levels of follicle-stimulating hormone (FSH) and luteinising hormone (LH).
On top of this, your male hormone levels might be higher than usual. This disrupts your menstrual cycle and you might get fewer periods than usual. Or you might not get any periods at all (amenorrhea).
Check your hormonal balance and learn if you might have this condition with our PCOS blood test.
Our vitamin D supplements can help improve testosterone levels and regulate your menstrual cycle if you suffer from PCOS.
What causes PCOS?
Truth be told, it’s not known what exactly causes PCOS. But there are a couple of things that can increase your chances of having it.
Your weight
If you’re overweight or obese it can increase the inflammation in your body. More evidence is needed, but inflammation is thought to increase your levels of male hormones — which can affect your ovaries and the hormones they produce.
Your insulin levels
High levels of insulin (a hormone that helps control your blood sugar levels) can cause you to produce too many male hormones.
Genes
PCOS tends to run in families so your genes might play a role. If a close relative has PCOS and you have some symptoms it’s worth looking into.
It’s clear that your hormonal balance has a big part to play but this can be influenced by a lot of different things.
What are the symptoms of PCOS?
Typically, the signs and symptoms of PCOS will start to show in your late teens/early twenties. These include:
- irregular or absent periods
- heavy bleeding when you have a period
- excessive hair growth — commonly on your face, back, buttocks, or nipples
- hair loss on your head or thinning hair
- weight gain
- oily skin and acne
- headaches
- difficulty getting pregnant — most people with PCOS can still get pregnant
Risks of PCOS
PCOS is also linked to an increased risk of long-term conditions, including:
- high blood sugar
- type 2 diabetes
- high cholesterol
- high blood pressure
- heart disease
You might also be more prone to anxiety and depression.
How to test for PCOS
Many people have PCOS but don’t know it. So if you think you might have this condition it’s important to get it checked.
Since PCOS is based on three main features (irregular periods, high levels of male hormones, and polycystic ovaries) diagnosing it will usually involve:
- questions about your menstrual cycle — so it’s a good idea to track your period and symptoms on an app (like Moody Month or Clue)
- a PCOS blood test to check your hormone levels — especially your levels of male hormones like testosterone
- an ultrasound scan — to check if your ovaries have a lot of follicles in them
Only two of these need to be present for your doctor to make a diagnosis, so you might not necessarily need an ultrasound scan.
Since PCOS can increase your risk of insulin resistance, diabetes, and high cholesterol, additional tests might be carried out to check your levels. For example, they might check your:
- fasting insulin levels
- HbA1c levels — your average blood sugars over the last three months
- lipid profile — your cholesterol and triglyceride levels
How to manage PCOS
If you’re diagnosed with PCOS, your GP or a specialist (like a gynaecologist or endocrinologist) will work with you to help manage your symptoms.
While you can’t cure PCOS, there’s a huge amount you can do to manage your symptoms.
Diet and lifestyle
If you’re overweight or obese, losing weight can be incredibly effective at reducing your symptoms and your long-term risks.
A low glycaemic index (low GI) diet has been shown to be one of the best types of diets to follow — even if you don’t need to lose weight. This means getting carbohydrates from low GI foods like fruits, vegetables, and whole grains.
Exercise is also really helpful — again, even if you don’t need to lose weight. Aim for at least three 30 minutes moderate-high intensity sessions a week. Exercise can increase your insulin sensitivity (how sensitive your cells are to insulin).
Supplements
Vitamin D supplements might help balance your hormones and improve your PCOS symptoms. Keep in mind that some supplements can interfere with medication used to treat PCOS.
Before taking a supplement, make sure to speak with a health professional.
Medication
If your symptoms are more severe, your GP might give you medication to help. Commonly prescribed medications include:
- an oral contraceptive (the pill) — balances your hormone levels
- Clomifene — encourages ovulation
- Metformin — improves your insulin sensitivity
Surgery
A procedure called laparoscopic ovarian drilling (LOD) can help with PCOS, especially if you’re having fertility problems. This is when heat or laser is used to destroy tissue in your ovaries. This can correct your hormone imbalances, allowing your ovaries to function normally.